Family Pathways to Care
How can City agencies coordinate referral pathways for public mental-health services to better support healthy child development and well-being?
Partners & Funders
The Project
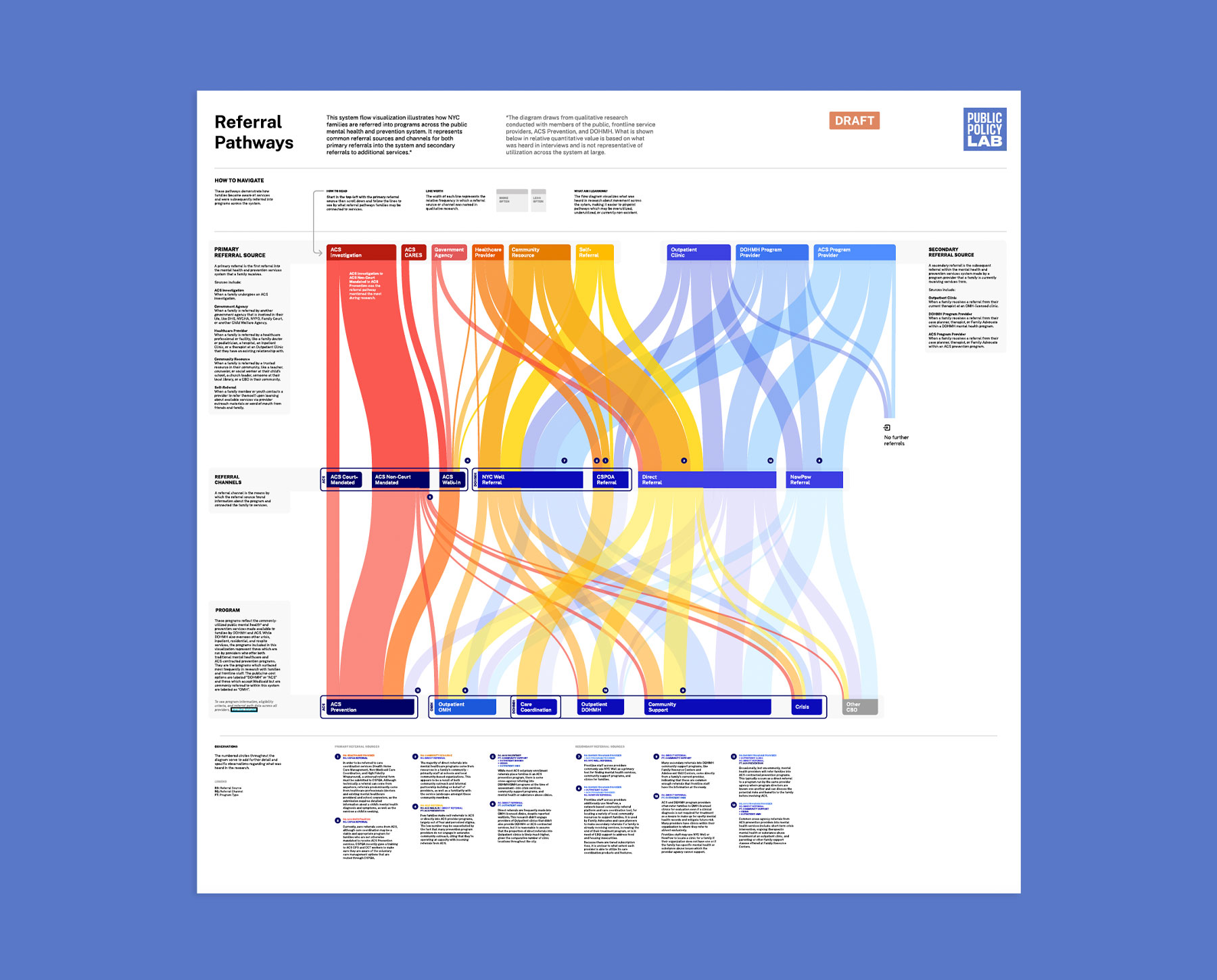
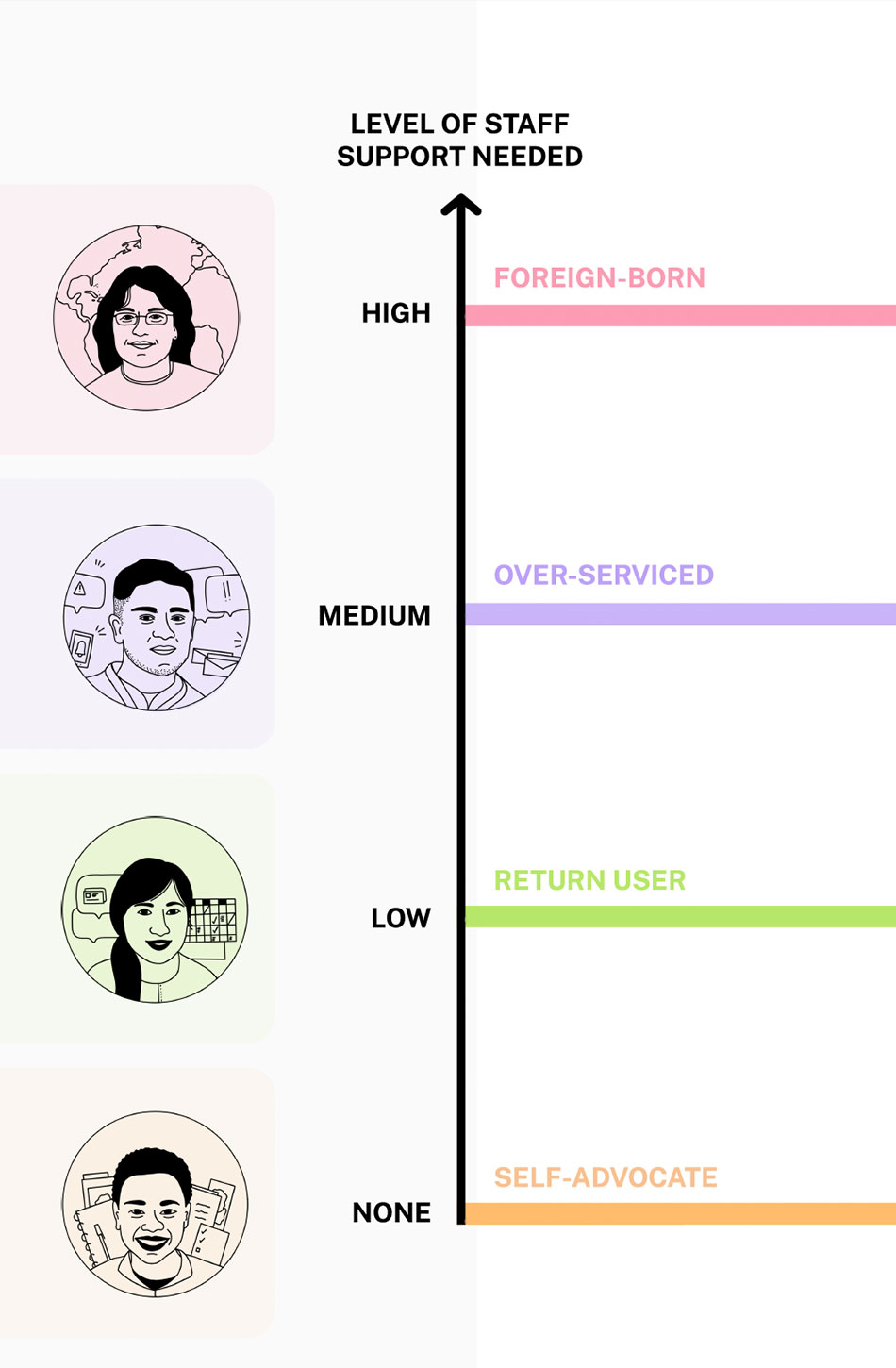
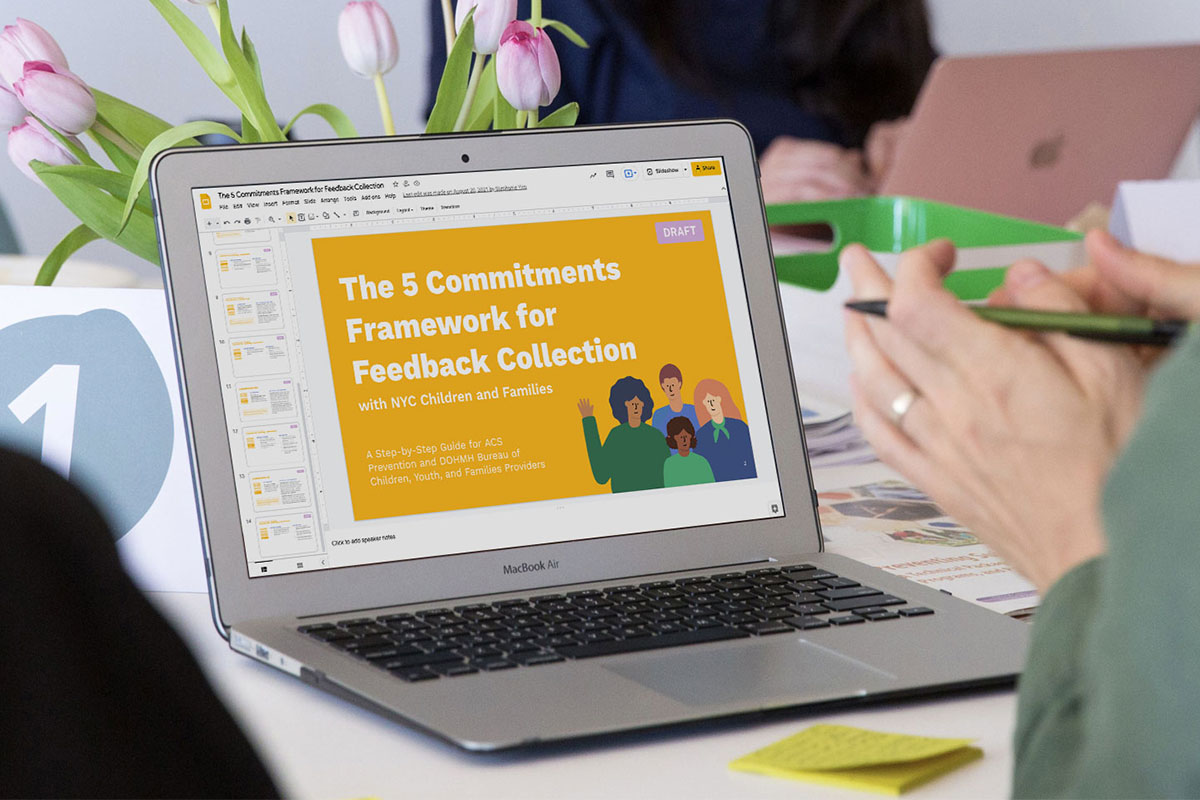
A variety of therapeutic and prevention services are available to low-income New Yorkers; however, these systems aren’t coordinated across City agencies. PPL partnered with New York City’s health department and child-welfare agency to understand what families need for comprehensive mental-health care and to improve inter-agency referral pathways.
The Outcome
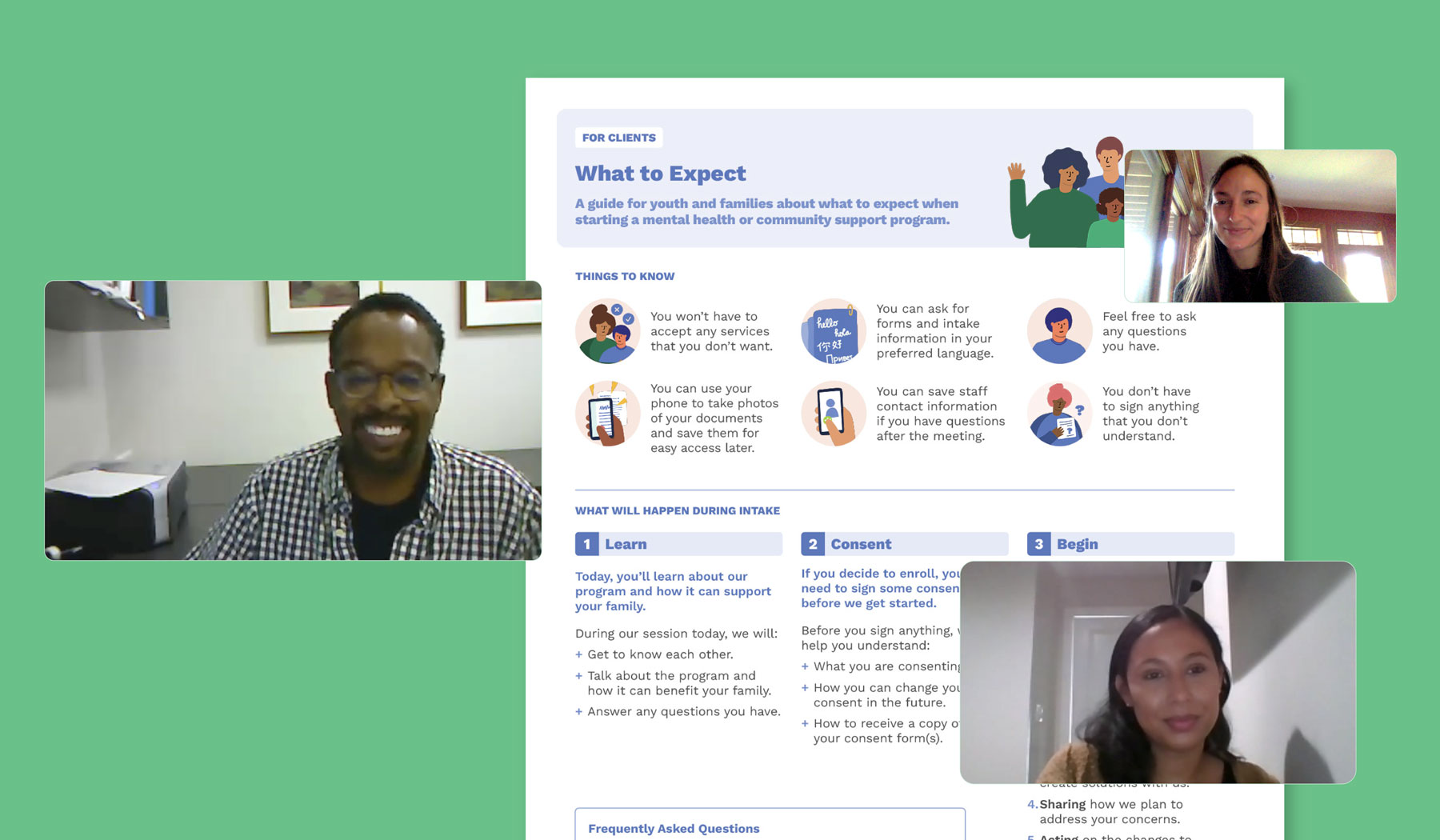
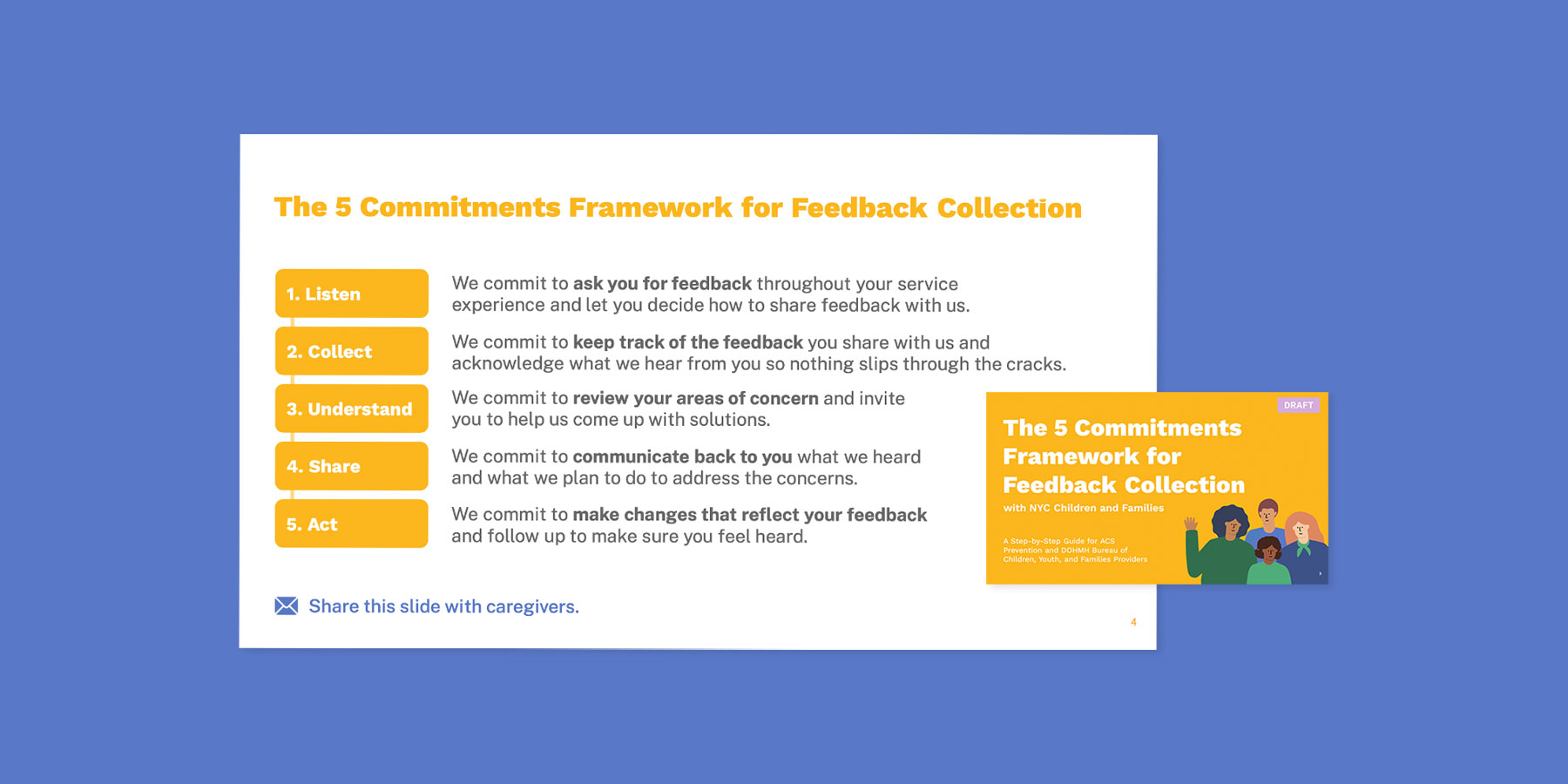
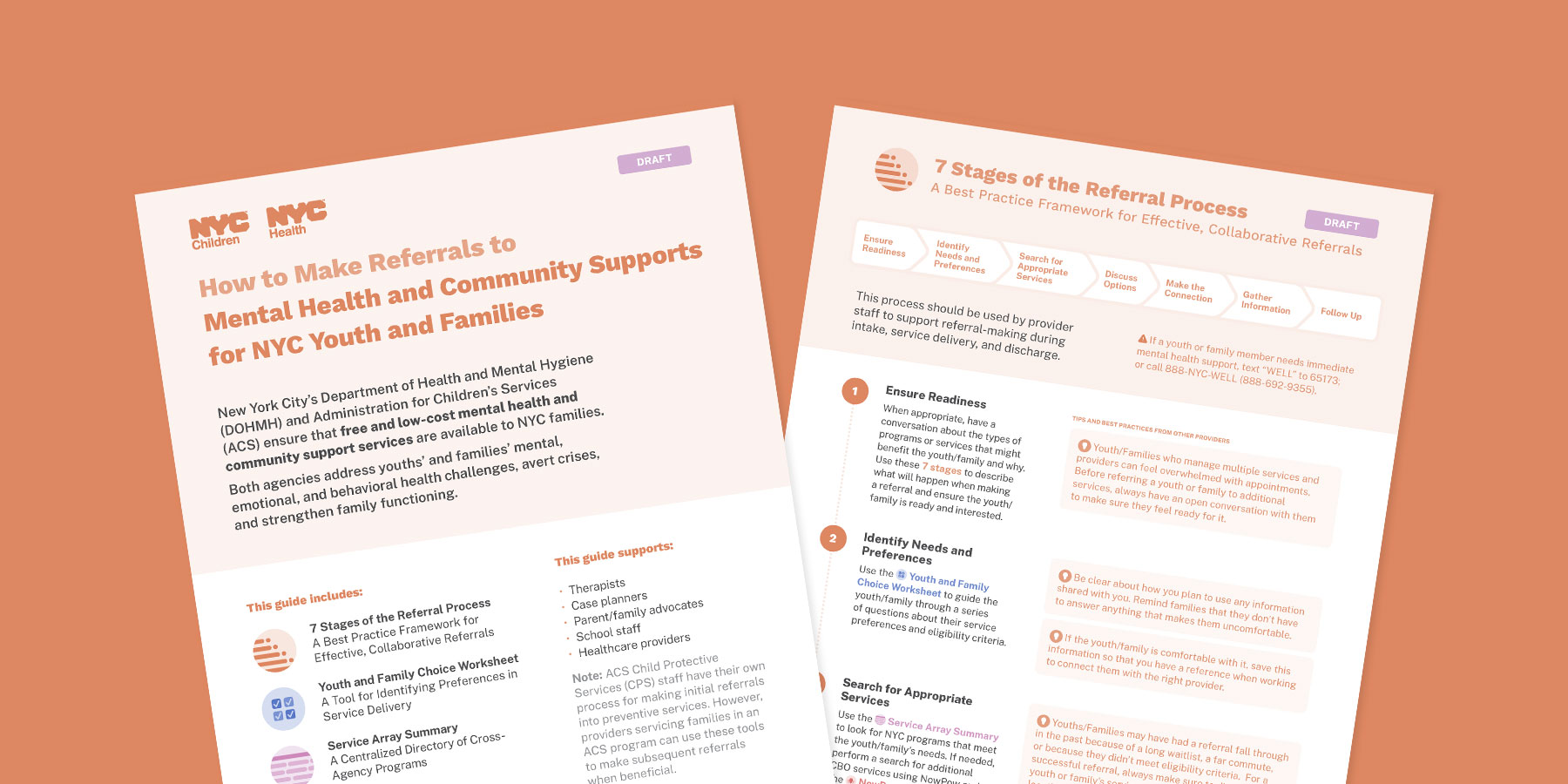
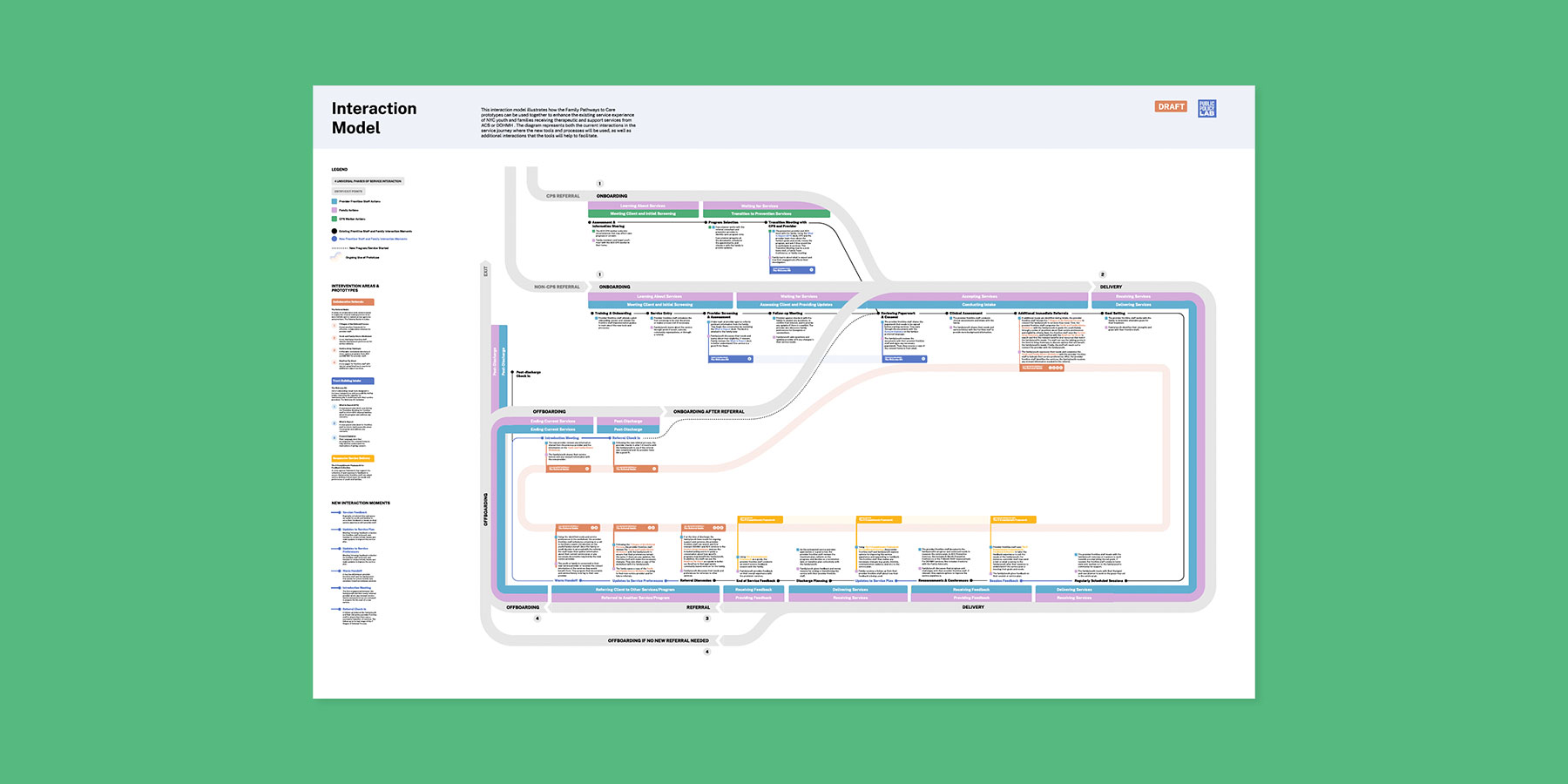
In collaboration with family members, City staff, and a cohort of service-providing nonprofits, we co-created and piloted a series of service delivery and operational tools designed to improve trust and coordination across three critical service touchpoints: intake, feedback, and referrals. These products are being rolled out to providers that serve thousands of families across New York City.
Family Pathways to Care
How can City agencies coordinate referral pathways for public mental-health services to better support healthy child development and well-being?
Partners & Funders
The Project
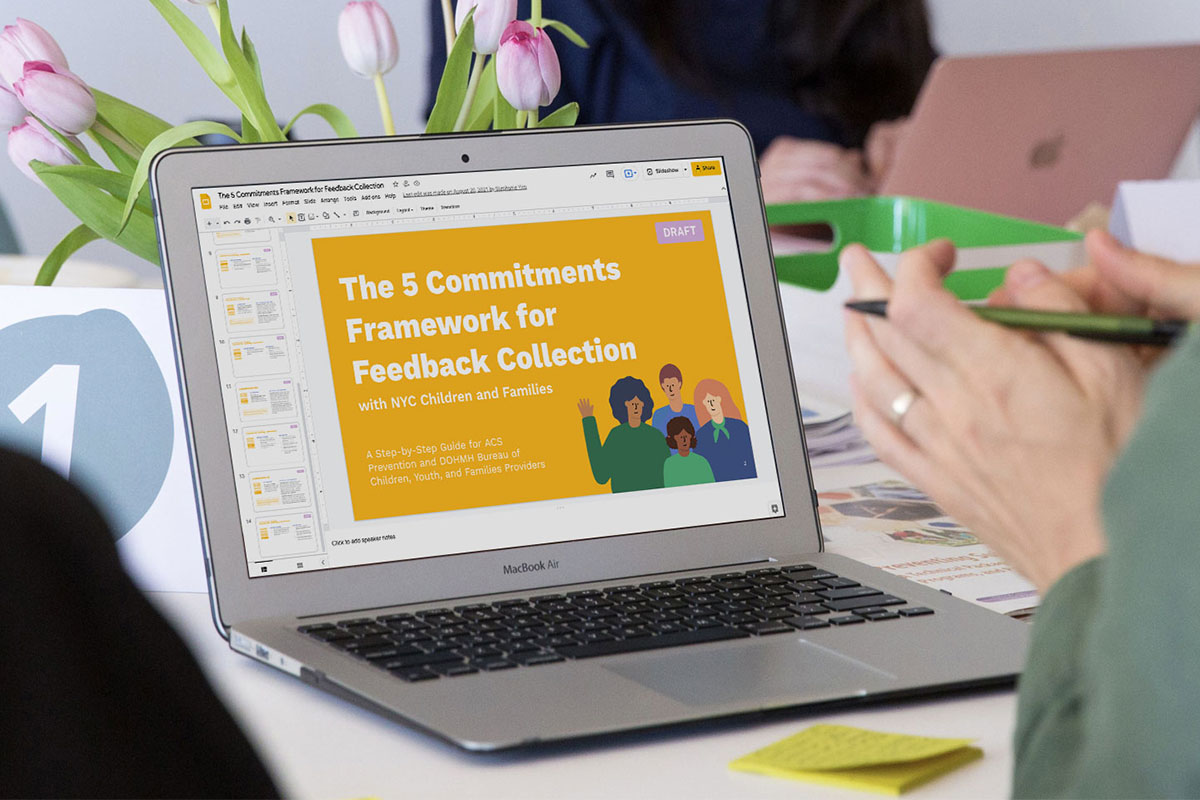
A variety of therapeutic and prevention services are available to low-income New Yorkers; however, these systems aren’t coordinated across City agencies. PPL partnered with New York City’s health department and child-welfare agency to understand what families need for comprehensive mental-health care and to improve inter-agency referral pathways.
The Outcome
In collaboration with family members, City staff, and a cohort of service-providing nonprofits, we co-created and piloted a series of service delivery and operational tools designed to improve trust and coordination across three critical service touchpoints: intake, feedback, and referrals. These products are being rolled out to providers that serve thousands of families across New York City.